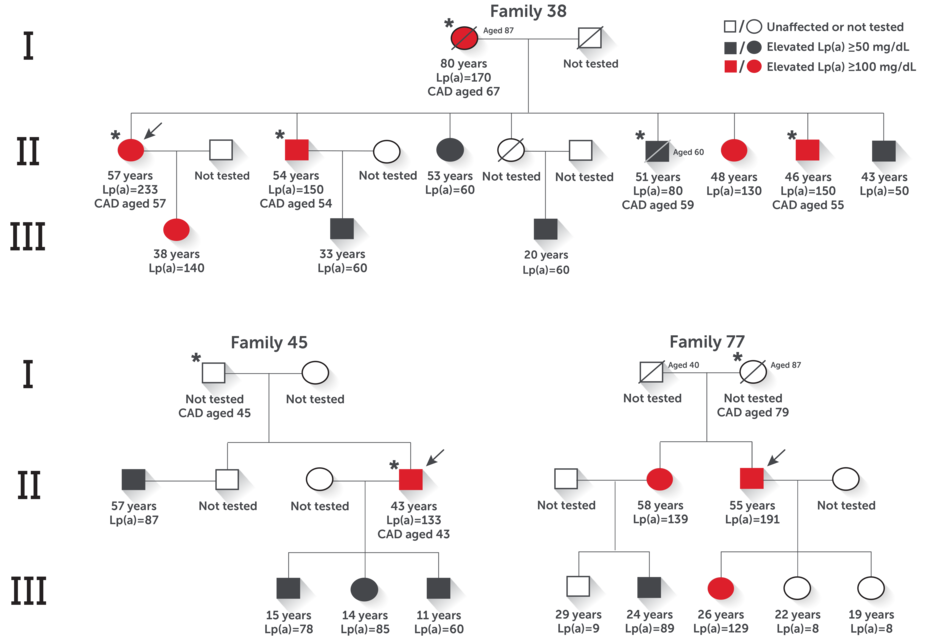
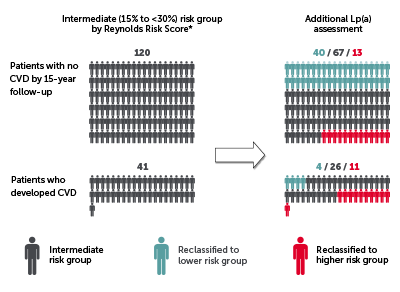
An elevated Lp(a) result can help inform an assessment of overall cardiovascular risk1-4
An elevated Lp(a) result provides an opportunity to monitor, identify, and initiate or intensify management of other cardiovascular risk factors1-4
For people with elevated Lp(a), monitoring and/or management of a patient's other cardiovascular risk factors such as hypertension, HbA1c, hyperglycemia, coronary calcium, high LDL, or low HDL are especially important.5-11