The National Lipid Association (NLA) recommends testing all of your adult patients for elevated Lp(a)† at least once1
Cascade screening of first-degree relatives of patients with elevated Lp(a) is also recommended to identify additional individuals at risk1
Early, more intensive risk-factor management, including lifestyle modification and lipid-lowering therapy to reduce LDL-C levels should be considered for high-risk patients1
†Elevated Lp(a) levels defined as ≥50 mg/dL or ≥125 nmol/L.1
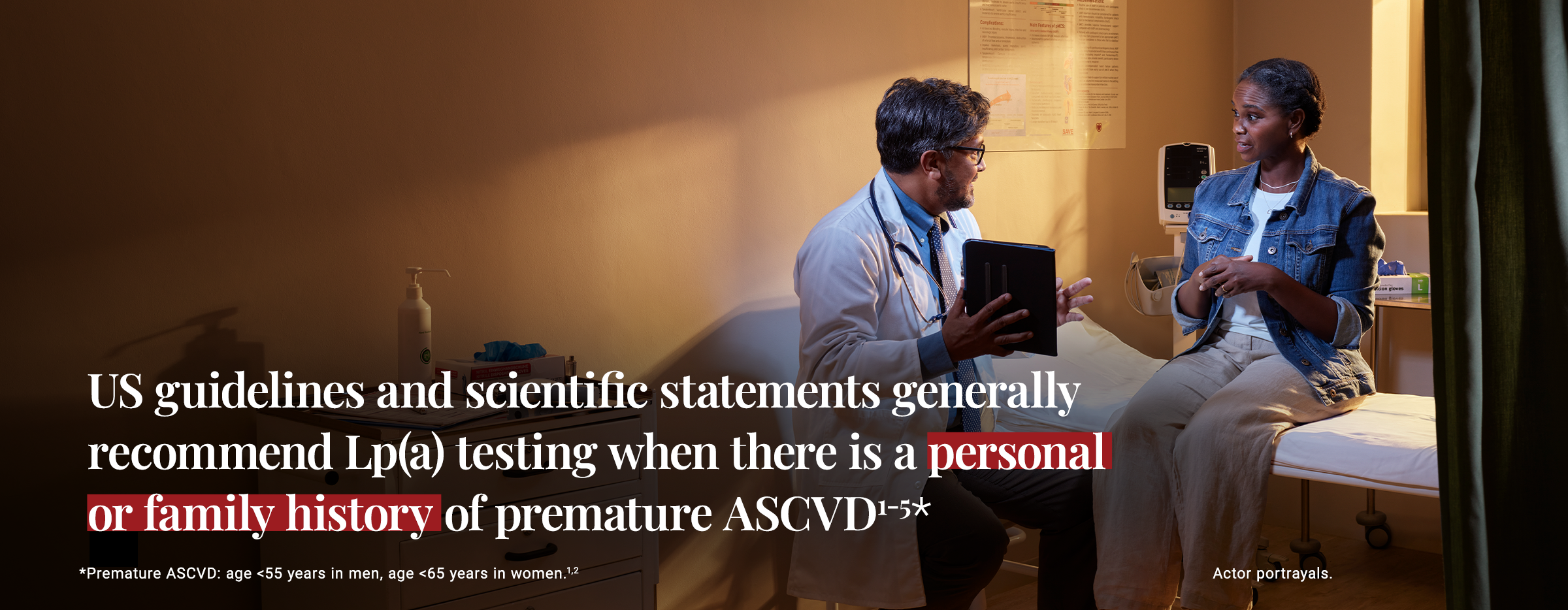
The American College of Cardiology (ACC) and American Heart Association (AHA) recommend an Lp(a) test for patients with a personal or family history of premature ASCVD1-5
Summary of US Statements and Guidelines Includes1-5‡:
‡Synopsis of guideline recommendations from NLA, ACC, and AHA/ACC. The 2025 AACE Clinical Guidance indicates that Lp(a) testing may be considered for individuals at intermediate ASCVD risk who understand the potential additional cost of testing and value risk information ascertained from Lp(a) to inform a treatment decision.6
§NLA 2024 publication is a focused update to the NLA 2019 scientific statement. This update recommends measuring Lp(a) in every adult at least once.1,2
IIThe 2024 update to the 2019 NLA scientific statement recommends measuring Lp(a) in every adult at least once for cardiovascular risk assessment.1,2
¶AHA/ACC guidelines note that relative indications for the measurement of Lp(a) include “personal history of ASCVD not explained by major risk factors.”4,5
Lp(a) testing is currently available and can be added to your patients’ routine blood work7
Billable ICD-10 codes8 | CPT code9 |
|
|
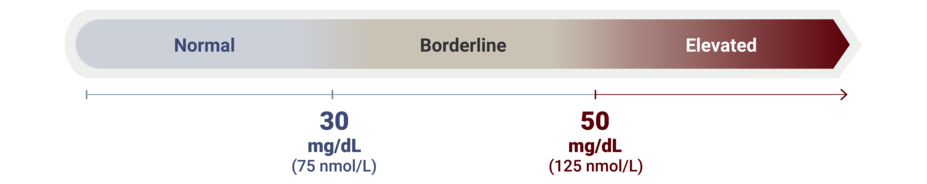
Lp(a) levels may be reported in mg/dL or nmol/L; either can be used to assess risk1
Increased cardiovascular risk (elevated Lp(a) level): ≥50 mg/dL (≥125 nmol/L)1
Borderline cardiovascular risk (borderline Lp(a) level): 30 mg/dL (75 nmol/L) to 49 mg/dL (124 nmol/L)1
Normal Lp(a) level: <30 mg/dL (75 nmol/L)1
A Discussion Guide is available that provides patient-friendly language to help you answer frequently asked questions about elevated Lp(a)
Lp(a) testing can help you manage the overall CV risk of your patients with premature CVD.1
ASCVD, atherosclerotic cardiovascular disease; CPT, Current Procedural Terminology; ICD-10, International Classification of Diseases, Tenth Revision; CV, cardiovascular; CVD, cardiovascular disease; LDL-C, low-density lipoprotein cholesterol; LLT, lipid-lowering therapy; Lp(a), Lipoprotein (a).
References: 1. Koschinsky ML, Bajaj A, Boffa MB, et al. A focused update to the 2019 NLA scientific statement on use of lipoprotein(a) in clinical practice. J Clin Lipidol. 2024;18(3):e308-e319. 2. Wilson DP, Jacobson TA, Jones PH, et al. Use of lipoprotein(a) in clinical practice: a biomarker whose time has come. A scientific statement from the National Lipid Association. J Clin Lipidol. 2019;13(3):374-392. 3. Writing Committee, Lloyd-Jones DM, Morris PB, et al. 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022;80:1366-1418. 4. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA /ASPC/NLA/PCNA guideline on the management of blood cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines Circulation. 2019;139(25):e1082-e1143. 5. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease. Circulation. 2019;140(11):e596-e646. 6. Patel SB, Wyne KL, Afreen S et al. American Association of Clinical Endocrinology Clinical Practice Guideline on Pharmacologic Management of Adults With Dyslipidemia. Endocr Pract. 2025;31(2):236-262. 7. Farzam K, Senthilkumaran S. lipoprotein A. In: StatPearls. StatPearls Publishing; 2022. 8. Engler RJM, Brede E, Villines T, et al. Lipoprotein(a) elevation: a new diagnostic code with relevance to service members and veterans. Fed Pract. 2019;36(suppl 7):S19-S31. 9. Quest Diagnostics. Lipoprotein (a). Accessed January 25, 2025. https://testdirectory.questdiagnostics.com/test/testdetail/34604/lipoprotein-a?cc=MASTER